Dirt-poor Mississippi Delta finds rural health care model in Iran, where far fewer infants die
By Shelia Byrd, APWednesday, June 2, 2010
Miss. looks to Iran for rural health care model
GREENWOOD, Miss. — Scratch-poor towns in the Mississippi Delta once shared more in common with rural Iran — scarce medical supplies, inaccessible health care and high infant mortality rates — than with most of the U.S.
Then things in Iran got better.
Since the 1980s, rural Iranians have been able to seek treatment at health houses, informal sites set up in small communities as the first stop for medical care, rather than an emergency room. They’re staffed by citizens, not doctors, and the focus is on preventive care.
Infant deaths have dropped from 200 per 1,000 births to 26. With the Delta’s rate 10 times worse than Iran’s, a group of volunteers is traveling to Iran this month to get a crash course in how health houses work.
“Why not try this?” asked Dr. Aaron Shirley, who has worked around the Delta for 40 years and is spearheading the effort to transform health care in a region where nearly three out of 10 infants die, residents are plagued by chronic illnesses, especially diabetes and heart disease, and few have health insurance.
The project is part of an agreement between Jackson State University, Shiraz University of Medical Sciences in Iran, the consulting firm Oxford International Development Group, and the Jackson Medical Mall, which provides health care to the poor in Mississippi’s capital. Shirley is chairman of the mall’s foundation board and the man behind its creation.
Five doctors from Iran participated in a conference on health disparities at the medical mall in October, and they were taken to the Delta to see the region’s plight firsthand.
“We’re hoping this project will create some kind of trust” between the two countries, said Mohammed Shahbazi, an Iranian-American who is a professor at Jackson State, said the health house exchange. “This is hope.”
The hitch is how the project would be funded. Shirley has been to Capitol Hill and approached some local leaders about the cost, which he estimates at $250,000 annually. But it’s hard to generate interest in something that involves sticky foreign relations, he said.
“We’re hoping to get somebody’s attention eventually. In the meantime, everything is being scrounged,” Shirley said.
Health house workers would be paid, but it’s unclear how. The care at the health house would be free to patients.
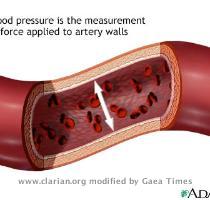
People who are ill can go to the health house where workers, who have been trained in medical basics such as taking blood pressure and recognizing symptoms of some illnesses, decide if patients need further treatment at a clinic or emergency room. Health house workers aren’t expected to have advanced medical skills and the houses would be affiliated with local clinics and hospitals.
James Miller, managing director of Oxford International Development Group consulting firm, is exploring whether the Obama administration’s federal health care law has funding provisions that can be tapped for the project. He said the law has provisions for community health centers and $15 billion over 10 years for preventive programs.
Miller said it’s been difficult to get federal money because the project doesn’t meet the criteria for program funding from the U.S. Health Resources and Services Administration.
“They’re funding programs like diabetes education and not the implementation of health systems, which is exactly what we’re trying to do,” said Miller.
Agency spokeswoman Tara Broido declined to comment on the health house proposal. She noted instead that a multiyear, $110 million agreement with the Delta Health Alliance has begun yielding results, including the expansion of a free clinic in Greenville.
Miller and Shirley contend their plan could save millions in health care dollars because people wouldn’t make unnecessary emergency room visits and preventive care averts costly hospitalizations for chronic diseases.
Health houses also could cut down on hospital readmissions, Shirley said. Patients often ignore the continuing care instructions they get when hospitals discharge them. Under the health house model, if the patient consents, instructions also would be given to health house workers, who would be responsible for helping the patient follow the regimen or contact physicians if that’s not happening.
More importantly, health houses would save lives, said Angela Cousin, a retired nurse who is one of the volunteers heading to Iran.
She recalled a dialysis patient who died because the woman was taking too much potassium. The patient didn’t realize that even though the pills looked different, they had the same ingredient.
“Some of the patients here are reading impaired,” and health house workers would notice those type of details, she said.
Shirley isn’t worried about liability issues because health house workers wouldn’t provide hands-on or invasive medical care. Hospitals and clinics connected to the health house would have their own malpractice insurance coverage, and besides, health house workers wouldn’t even apply bandages on their own, he said.
That doesn’t mean they couldn’t make a difference.
In an 11-county, predominantly black region of the Delta, the infant mortality rate is 281 deaths per 1,000 births. About 13 percent of the region’s population has diabetes. In Leflore County, where Greenwood is located, 42.4 percent of the 35,000 people live in poverty. Nearly 33 percent are obese and 11 percent have diabetes, according to state health statistics. Nine percent have cardiovascular disease.
There’s one hospital in Greenwood and three others in neighboring counties, serving much of the region.
Part of the problem with people seeking medical care is rooted in the culture: Some blacks still distrust white physicians, said Cousin, who is black.
There’s also a disconnect between health care providers and the community, said Dash Brown, a 26-year-old community activist with thick dreadlocks who lives in Baptist Town, a neighborhood in Greenwood known as the place where seminal bluesman Robert Johnson lived and died.
Brown said a health fair offering low-cost screenings was recently held near Greenwood, but it was on the 27th of the month. Organizers should have held the fair at the start of the month, he said, when people who receive public assistance usually get their checks.
“A lot of people are on a fixed income. At the end of the month, nobody has a $100 to spend on a health fair or any medical treatment,” Brown said.
Online:
Mississippi Health House Network: www.hchaweb.com
Tags: Child And Teen Health, Death Rates, Demographics, Diabetes, Diseases And Conditions, Greenwood, Health Issues, Health Statistics, Iran, Middle East, Mississippi, North America, Oxford, United States